MEET MARTI
Medical • Artificial • Real • Time • Intelligence
MARTI helps payers and at-risk providers by identifying patients at risk of costly health events, enabling proactive intervention for prevention and mitigation.
$100 saved per member per month
DeLorean AI’s medical AI, MARTI, reduces MLR (medical loss ratio) by as much as $100PMPM and increases revenue while enhancing the quality of care and extending patients’ lives.
Identify High-Risk Members
Dynamic Risk Stratification
Identify unknown patients
Transition Prediction
Tailored Care Recommendations
MARTI = Intervention & Prevention
85-87% prediction accuracy
Real science by real scientists
Led by Severence MacLauglin, Ph.D
CATALYZING VALUE-BASED CARE
Designed for Scale
ON PREM
Unparalleled scope
Depth of model
Interoperability
HEALTH BENEFITS
With the ability to better classify patient populations, assign risk, and predict disease state transitions, Medical AI directly leads to:
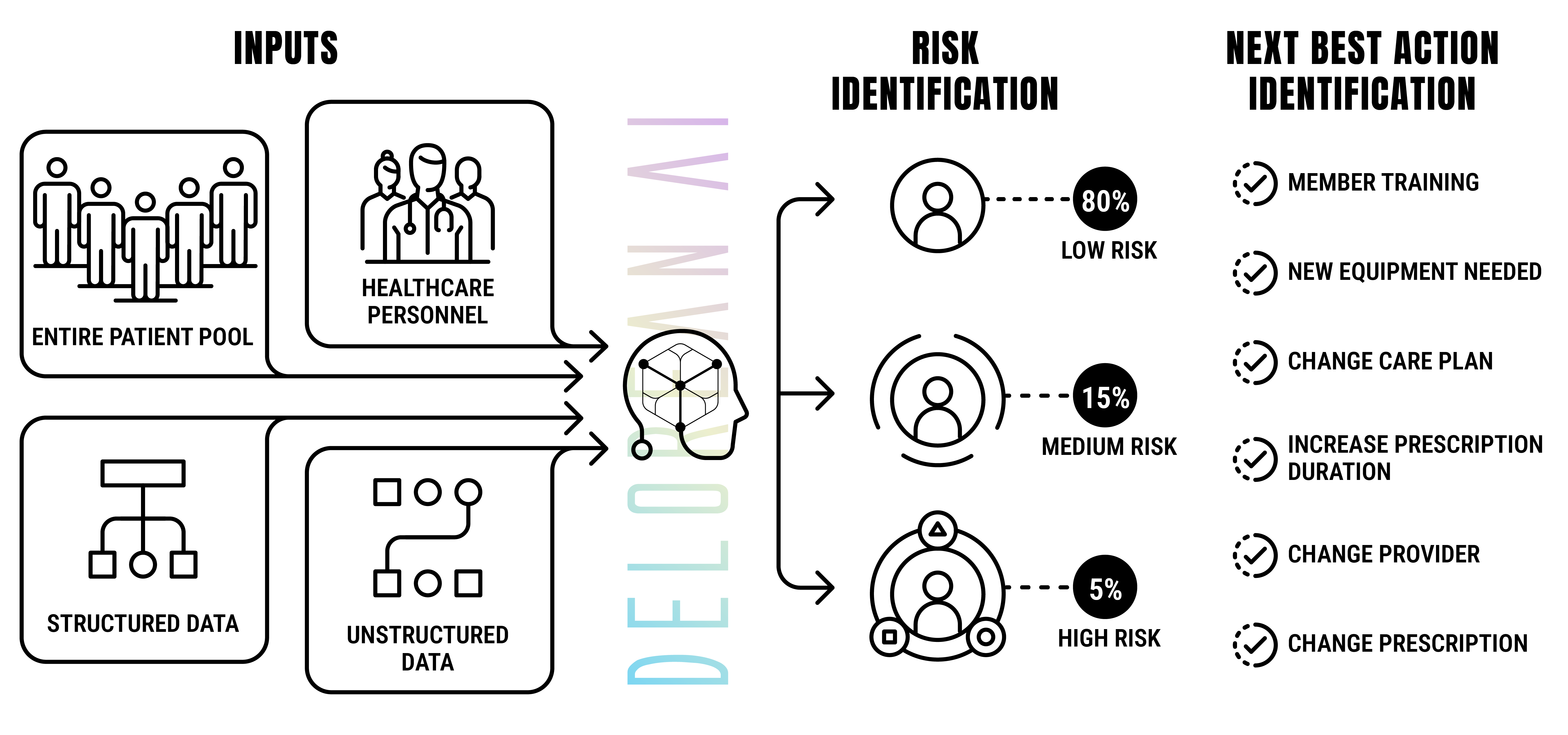
Hyper-personalized “Next Best Actions”
Gives clinical teams care pathway options to improve patient outcomes. MARTI is proven to optimize patient outcomes while reducing medical cost exposure.
Holistic Views
Earlier detection and diagnosis of diseases / illnesses
Improved disease / illness management
Halted disease progressions
MARTI delivers answers proactively providing predictions and recommendations
Before Patients seek care
Before Claims are submitted
Before major health events occur
Before Disease states are identified
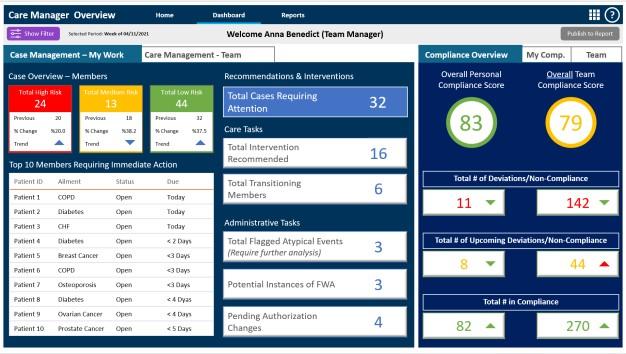
Easy to consume dashboards
ADDITIONAL BENEFITS OF LEVERAGING MARTI
Deferred treatment
“Sixty percent of surveyed clinicians indicated that deferred care led to an increase in complications, 30 percent reported an increase in mortality, and 55 percent noted an increase in self-medicating and forgoing necessary prescriptions.”
MARTI precisely identifies patients that are in deferred-care patterns and facing imminent events/transitions. By focusing care teams on these patients before they require intensive care, costly interventions can be avoided.
Aging Populations
“In the United States from now until the end of 2029, 10,000 people are estimated to turn 65 years old each day. Within this population the incidents of comorbidities increases significantly with more than 50% of older adults living with three or more chronic conditions (IJEPH).” – Xtelligent Healthcare Media: (September 6, 2022)
MARTI offers insurers and ACOs powerful tools to control costs as their member and patient populations age. Through precision identification of patients on the verge of transitioning to advanced and critical disease states, clinical teams can focus their resources on reducing and even preventing comorbidities.
Value Based Care
69% of employers and 61% of consumers said they prefer value-based care over fee-for-service models. – Emblem Health
Given the choice, employers and consumers both prefer value-based care systems. MARTI empowers both payers and providers to deliver on the ultimate promise of true healthcare – ensuring wellness.
Other AI services for Healthcare vs. MARTI
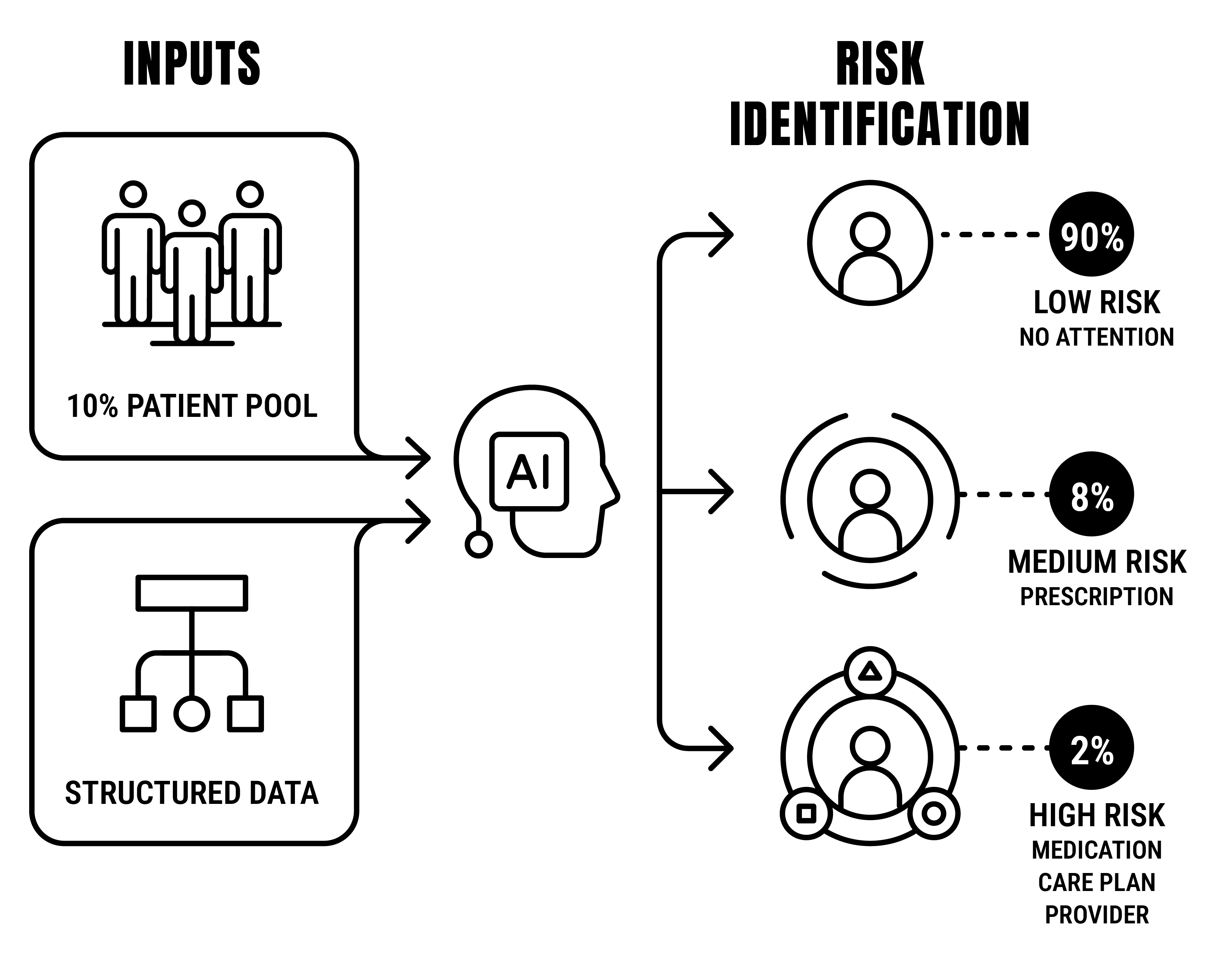
Other AI Services
Current AI solutions only use structured data and a portion of the available patient population to deliver broad-stroke analytics to inform users about what is going on.
the difference with MARTI
MARTI uses the entire patient population, structured and unstructured data, as well as supporting health information from personnel, EHRs, labs, etc. After performing classifications, MARTI produces predictions and next-best-action recommendations, to realize better care.
Care Modules for Chronic Illness Management
DeLorean AI currently offers four (4) modules that are ready to deploy for renal, diabetes, cardiovascular, and behavioral health. Note: our Respiratory AI is slated for release at the end of Q4 and High-risk Pregnancy in Q1 of 2024.
RENAL
RENAL
PMPY SAVINGS:
ESRD $15k / CKD $1200
DIABETES
DIABETES
PMPY SAVINGS:
Diabetes $2800 / Pre-Diabetes $500
CARDIAC
CARDIAC
$1000
Behavioral
Behavioral
PMPY SAVINGS:
Stat coming soon!
RESPIRATORY
RESPIRATORY
Coming in Q1 of 2024!